The purpose of this post is to contribute a very extreme case of shingles that challenges the notion that having shingles substantially increases your odds of developing Alzheimer’s Disease (AD).
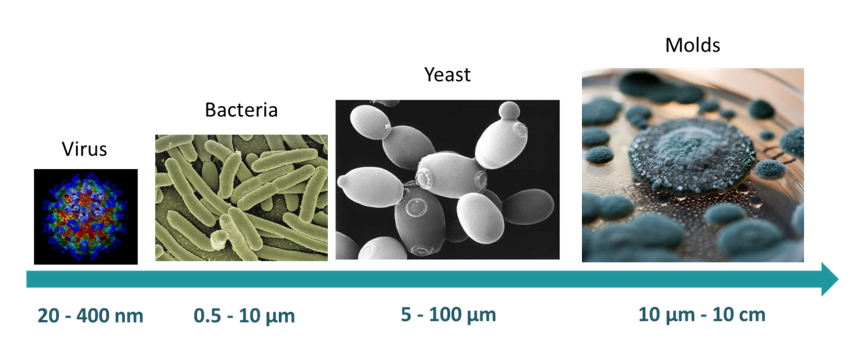
We agree that there is a connection between shingles and AD –they are both caused by microbes. Shingles: by a virus; and Alzheimer’s: by a bacteria or fungus as all three are microbial and capable of infecting the brain. But we disagree that AD and Shingles are caused by the same microbe.
——
Our Co-founder, Dr. Crandall could have been called the modern day Job [biblical reference] of the patient world. In that, if there was a side effect to anything, or if there was a chance something would go wrong medically – it would happen to him. And in this case, because he was on immune-suppressive drugs for so long, and because of his advanced age – the likelihood that he’d experience shingles was greatly increased.
Dr. Crandall and his doctors felt confident that he was protected from getting Shingles as he’d received the Shingles vaccine Zostavax.
But just after his 83rd birthday, he noticed a tingling sensation on his forehead above his left eyebrow. The tingling quickly moved to shocks that he tried to ward off by pressing hard on his skull. As the nerve signaling worsened, I called the pharmacist to see if any of his medications could cause this disturbing side effect. Of great concern was his new anti-inflammatory drug. Dr. Crandall was already convinced he was on to something because of his increased attention span, recall and processing speed (another blog post will delve into this more comprehensively). But unfortunately, his hopes were dashed when his pharmacist felt this new symptom was Shingles – along the Left Trigeminal Nerve branch – and was directly related to his drug change.
At first Dr. Crandall said he could take the pain and burning as a trade-off for his exciting cognitive improvements. But as the pain became debilitating, he was left no other choice than to go to the hospital where his new treatment was stopped.
Now this was no ordinary case of shingles. Dr. Crandall was diagnosed with both Herpes Zoster Ophthalmicus (HZO)- and Post Herpetic Neuralgia (PHN). Both of which are considered rare, but increase in incidence with age.

After 7 days on a morphine drip, then 29 days in the TCU [and an accidental opioid overdose by his nurse], Dr. Crandall was able to return to his home – but for the first time in his life he needed support. This was a huge blow to his independence and represented a new cognitive milestone. It was as if his cognitive decline went from zero to sixty in just two short months. Before Shingles, he’d been living successfully on his own. After Shingles, Dr. Crandall found himself needing help with the simplest of daily chores. And driving? His prize Lexus would never leave his garage again.
Had Dr. Crandall not been experiencing Mild Cognitive Impairment (MCI) prior to shingles, we would have recalled that horrific shingles experience and directly attributed all the AD pathology found on autopsy to the herpes virus. But that wasn’t the case. The fact was, he had been experiencing MCI for at least 8 years prior to contracting shingles. [Good to know: Dr. Crandall started experimenting with steroids three years into his MCI which dramatically slowed the disease progression and is why his doctors looked for other medical conditions other than AD that could explain his cognitive impairment. Meaning by the time he developed Shingles, he had been on steroids for about 5 years.]
So, because of his prior MCI, we are portraying the HZO viral infection as a co-infection that created unique brain damage on its own. In fact, DEC’s autopsy identified substantially more temporal lobe atrophy on the same side that was crippled by the herpes zoster virus. [It will be interesting to see if there is more AD pathology on the left hemisphere. We will report on that once we know.] This pathological observation finally explained why, before shingles, massive doses (60-100 mg) of steroid allowed him to return to his early 70’s baseline, but after shingles no level of steroid was able to get him even close. And for all the skeptics: no, there was no sign of seizure or stroke that could have accounted for the amount of localized damage observed at autopsy. Instead, we are compelled to believe that the herpes virus is what caused the damage. As supported by one of many studies connecting HZO to brain tissue damage.
And because Dr. Crandall was “cured” of the herpes infection through IV Valacyclovir followed by oral dosing for two additional years, and because anti-viral medications have no effect on bacterial infections, he was left with just his primary infection that continued its slow smolder until he finally succumbed to that disease process in his 85th year.
Disclaimer
No content on this site, regardless of date, should ever be used as an absolute substitute for direct medical advice from your doctor or other qualified clinician. This article should be viewed as advice that is based on current research regarding the potential to slow and possibly prevent Alzheimer’s Disease.
Copyright © 2022 Curing Alzheimer’s Disease [EIN #88-3154550] All Rights Reserved. This information is not designed to replace a physician’s independent judgment about the appropriateness or risks of a procedure for a given patient. Always consult your doctor about your medical conditions. Curing Alzheimer’s Disease.com does not provide medical advice, diagnosis or treatment. Use of the site is conditional upon your acceptance of our terms of use.
Alzheimer’s Disease, Curing Alzheimer’s Disease, Mild Cognitive Impairment, Alzheimers and Herpes Zoster, Alzheimers and bacteria, Steroid responsive cognition, DEC Legacy Lab


